We use cookies to help provide you with the best possible online experience.
By using this site, you agree that we may store and access cookies on your device. Cookie policy.
Cookie settings.
Functional Cookies
Functional Cookies are enabled by default at all times so that we can save your preferences for cookie settings and ensure site works and delivers best experience.
3rd Party Cookies
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Menopause & Perimenopause
By Dr Rhianydd McGlone, Langley House GP and British Menopause Society Menopause Specialist
What is the menopause?
Menopause is the cessation of a woman’s menstrual cycle. The typical age of menopause in the UK is 51 years, and most women become menopausal between the ages of 45–55 years. Menopause is defined as the cessation of periods for 1 year. Before periods come to a complete stop they often change, as the ovaries struggle to work as regularly and reliably as they did in the past. Hormone levels fluctuate during this transition, and in particular there is a reduction in the amount of circulating oestrogen (produced by the tiring ovaries). Periods themselves may become lighter, heavier, or variable in volume and occur at different intervals of time. Hormone levels fluctuate in a way that the body is not used to and this, in combination with a declining level of oestrogen, can cause a variety of symptoms.
Symptoms women may, or may not experience:
- Hot flushes
- Night sweats
- Vaginal dryness and discomfort during sex
- Difficulty sleeping
- Low mood or anxiety
- Problems with memory and concentration, ‘brain fog’
- Reduced sex drive.
- Worsening symptoms of premenstrual syndrome (symptoms before a period)
- New or worsening migraines
- Joint stiffness, aches and pains
- Recurrent urinary tract infections
- Palpitations
The time interval in which women experience symptoms before their periods stop is called the perimenopause and can last months to years. On average, symptoms of the perimenopause and menopause resolve approximately 4 years after periods stop completely, as the body eventually adapts to the constant lower level of oestrogen. The term postmenopause is used to describe the time after the cessation of periods for over 1 year i.e. after the menopause takes place.
It is considered ‘early’ to enter the menopause (periods stopping completely) between the ages of 40-45years, and ‘premature’ to enter it before the age of 40 years. Some women enter the menopause early or prematurely due to the side effects of medication, or as a result of surgery.
Menopause isn’t just about symptoms
Becoming menopausal is associated with increased health risks, and this is much better understood now than it was in the past. Low oestrogen levels lead to an increase in cardiovascular (heart) disease, osteoporosis (weak bones) and urinary tract infections (UTIs).
But it’s not all bad news! The Chinese refer to the menopause as a woman’s ‘second spring’. Thanks to advances in nutrition, sanitation, medicine and other public health measures, the average life expectancy for women in the UK is now 83 years. Woman may spend over a 3rd of their lives in the menopause and it is an opportunity to re-evaluate, re-prioritize and nurture the things that are most important to us, including our health.
How to diagnose the menopause or perimenopause
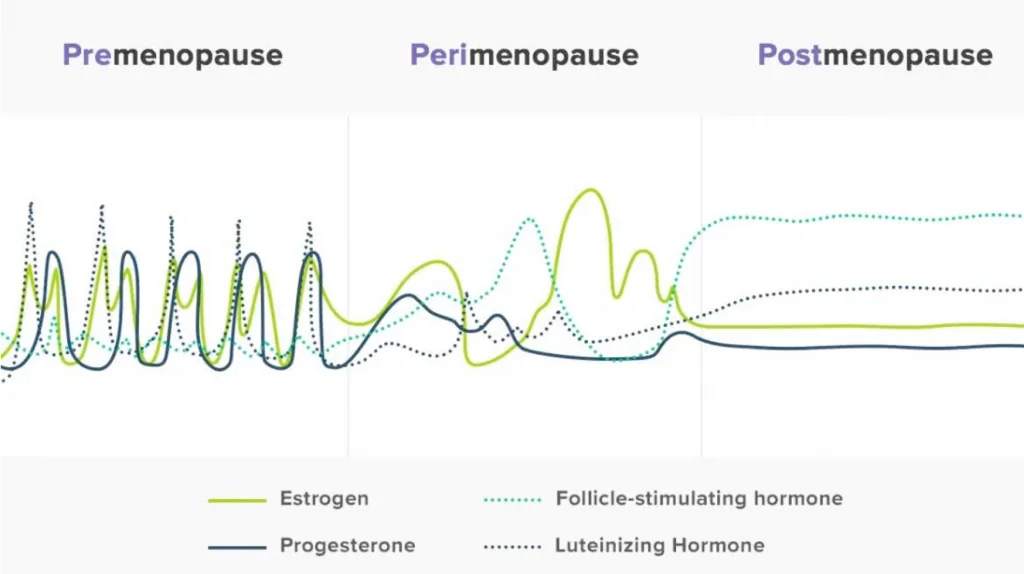
For most women, the diagnosis of perimenopause or menopause is a clinical one. The diagram above highlights the fluctuating hormone levels women experience. Taking blood or urine samples in a bid to diagnose the perimenopause or menopause is unreliable and largely unhelpful. Furthermore, hormone levels do not correlate well with symptoms: two women with the same hormone level can have very different symptoms, and the decision to offer treatment should be based on the nature of the symptoms, rather than the blood hormone level. Although private providers of menopause care may advocate blood tests, the NHS does not routinely provide this as there is no evidence that it is helpful in coming to the right decisions about treatment.
Treatments of Menopause and Perimenopause
Symptoms of the menopause, and the increased risk of certain diseases, can be improved with lifestyle changes and medication.
Lifestyle
It is more important than ever to try to lead a healthy lifestyle in the perimenopause and menopause. Activities that we could ‘get away with’ in our 20s and 30s, catch up with us in our 40s and 50s. Women will struggle to tolerate late nights, excess alcohol, smoking, and a lack of exercise, and these are the first areas that need addressing if perimenopausal or menopausal symptoms are troublesome. Measures include a healthy diet, regular exercise, managing stress, avoiding alcohol, stopping smoking and trying to maintain a healthy weight. All these lifestyle improvements reduce the risk of heart disease, bone thinning and cancer.
Online help with lifestyle improvements can be found free of charge
Local help with lifestyle improvements can be found free of charge
Hormone Replacement Therapy (HRT)
HRT involves topping up a woman’s supply of oestrogen with the intention of relieving symptoms. It is the most effective way to relieve symptoms, and has been proven to reduce the risk of heart disease and bone thinning (osteoporosis).
The principle hormone replaced is oestrogen. This is usually given as estradiol on the NHS, a chemical that is derived from plants, but which is molecularly identical to human oestrogen. This similarity is termed ‘body identical’. Women can receive oestrogen via mouth or via the skin (transdermal). There are advantages and disadvantages of each route which will be considered later.
If a woman still has a uterus (womb), it is necessary that she take a second hormone in her HRT called progesterone. Oestrogen and progesterone work in synergy in the womb during the normal menstrual cycle. Oestrogen encourages the lining of the womb to grow (thickening in anticipation of pregnancy), while progesterone organized that growth and keeps it uniform. A lowering of progesterone levels later in the menstrual cycle induces the lining of the womb to shed and bleed. It is helpful to think of progesterone like the ‘cement’ that binds the oestrogen ‘bricks’ together and ensures the lining does not overgrow. When the cement is removed in the later stages of the menstrual cycle, the wall crumbles and a period ensues. Giving oestrogen (bricks) without progesterone (cement) can lead to disorganized growth of the lining of the womb, with an increased risk of irregular bleeding and uterine cancer. Progesterone must always accompany oestrogen HRT.
Progesterone can also be given in a variety of ways (patch, oral or directly into the womb), and can be body-identical or synthetic. Synthetic progesterone is called progestogen. Body-identical or synthetic progestogens have different risks and benefits, and these are further considered below.
How is oestrogen (estradiol) best taken?
Taking oestrogen by mouth is associated with a small increased risk of blood clots and stroke, which is similar to the risks from taking the combined oral contraceptive pills. Taking oestrogen through the skin (transdermal) is not associated with these risks, and should be the first-line route of administration for women over the age of 60 years, or those with other health problems such as obesity, diabetes and high blood pressure. Transdermal oestrogen comes in gels, patches or a spray. The choice of product is mainly determined by convenience of application, or current availability. Some women find that their symptoms are better controlled by one transdermal product rather than another. This is likely due to differences in absorption and is impossible to predict. A small number of women find benefits from oral HRT only, seemingly unable to absorb estradiol through their skin.
- Patches are applied to the buttock, thigh of lower abdomen and come in a range of doses: 25mcg, 50mcg, 75mcg or 100mcg. They are designed to remain in place for 3-4 days at a time and should be changed twice weekly. They do not need to be removed for bathing or swimming. Patches are a very convenient option for a lot of women, and are particularly good for women with hormone sensitive migraines, as the drug delivery is very constant.
- Gels are similar in texture to alcohol hand gel, and a metered dose or ‘pump’ is rubbed in to the outer arms and inner thighs. Women can increase their dose by increasing the number of pumps, up to a maximum of 4 pumps daily. Some women prefer a daily application product such as a gel, but others find it sticky or time consuming to wait for it to dry before dressing.
- An estradiol spray is also a once daily application, and is similar to an odourless perfume. It is squirted on to the skin of the forearm or inner thigh (in the same area each day) and dries within a few minutes. The dose can be increased up to a maximum of 3 sprays daily.
Why choose one progesterone product over another?
Some synthetic progestogen products provide contraception and are also helpful in treating problematic periods. These advantages should be taken into consideration when choosing a HRT product.
For many women, particularly those who are still having regular or problematic periods, the Hormonal Intrauterine System (IUS) is a popular way to receive progestogen. An IUS provides contraception, bleed control, protects the lining of the womb, and results in low overall progestogen absorption. Most women can have this device fitted for free at the surgery and it lasts for 5 years.
For women who do not wish to have an IUS fitted, there are 3 alternative options: body-identical progesterone by mouth, synthetic progestogen by mouth, or synthetic progestogen via a patch.
Why do some women take progesterone all the time, while others only take it for a proportion of the month?
In women who are still menstruating, or who have only recently stopped, progesterone is given in a cyclical manner in keeping with a woman’s natural cycle. This means taking the progesterone for 2 weeks out of every month. This regimen maintains a regular bleed. In women who are no longer bleeding, progesterone can be taken daily and should not induce bleeding. For women in-between (having some, but not frequent bleeds) a clinician will consider which regimen is preferred. If progestogen is delivered directly in to the womb it is given continuously regardless of whether a woman is still having periods or not.
Other than symptom control, what are the advantages of HRT?
HRT has been proven to reduce the risk of heart disease and the risk of bone thinning. There are likely to be many other benefits too. One study found that HRT reduced the risk of death from all causes by 45% in women who took HRT under the age of 65 years, compared to women who did not. It is also worth noting that the benefits of HRT depend on when it is initiated. Heart benefits of HRT are only apparent in women who commence HRT within the first 10 years of their menopause, and before they develop heart disease.
What are the risks of HRT?
The risks of HRT are minimal, and for most women the advantages of symptom control and reduction in the risk of heart and bone disease outweigh the risks.
A combination of oestrogen and progestogen HRT is associated with a small increase risk of breast cancer, but this small risk is comparable to the risk of breast cancer associated with smoking, drinking 2 units of alcohol a day or taking the combined oral contraceptive pill. Being overweight (body mass index >30) confers a much greater risk of breast cancer than HRT does. Exercising for 2 and a half hours a week reduces the risk of breast cancer. Putting the risk of breast cancer from HRT into context with the risk from other lifestyle decisions is important, but something which is not often reflected in media coverage of the breast cancer risk from HRT.
Visit Women's Health Concern to view the factsheet on Breast cancer risk factors
HRT is also associated with a very small increased risk of ovarian cancer.
What are the side effects of taking HRT?
Any symptoms that occur as a result of taking HRT are normally short-lived and resolve after a few months. A change of route or dose can facilitate this. Symptoms may include breast tenderness, mood changes, bloating and nausea.
What if I have a family history of breast cancer?
HRT is not completely contraindicated in women with a family history of breast cancer. It is important to recognize that woman with a strong family history of breast cancer are already at increased baseline risk. Adding HRT will increase their risk a little more, but the proportion of additional risk is small and should be balanced against the potential benefits of HRT. Women with a strong family history should discuss their risk with a clinician. Some women are eligible for more frequent breast cancer screening if considered to be at moderate or high risk of breast cancer.
Are some types of HRT safer than others from a breast cancer point of view?
Oestrogen only HRT (without progesterone or progestogen) is not associated with an increased risk of breast cancer, but this is not an option for women with a uterus (womb) due to the increased risk of uterine cancer.
The combination of oestrogen and progestogen in HRT is responsible for the increased risk of breast cancer. Different progestogen preparations confer different levels of risk. A body identical progesterone appears to be the safest preparation, and may not increase the risk of breast cancer for the first 5 years of use. Body identical progesterone is only available as a tablet. This can be combined with oestrogen in the form of a tablet, gel, patch or spray. Body-identical progesterone is available on the NHS.
Women are encouraged to check their breasts monthly and take part in routine NHS breast cancer screening, whether they take HRT or not. No additional monitoring is required for women taking HRT. Although combined HRT (oestrogen and progestogen) may increase the risk of having breast cancer, there is no increased risk of dying from breast cancer in women who take HRT.
If body-identical progesterone is safest, why might some women choose a synthetic progestogen?
Synthetic progestogen can offer contraception and improved bleeding, and these advantages may be a higher priority for some women than the lower risk of breast cancer.
What are other considerations that might guide HRT regimen choice?
An increased risk of blood clots or stroke necessitates taking oestrogen through the skin (transdermal). Transdermal oestrogen is less likely to increase the risk of blood clots or stroke, and can still be considered for use in women who have a history of these conditions. Women over the age of 60 years, or with other chronic health conditions such as diabetes, obesity or high blood pressure, should also take oestrogen through the skin.
Women with hormonal migraines tend to find that transdermal oestrogen is less likely to precipitate headaches. Patches or a spray are generally considered best.
For women who have already been diagnosed with bone thinning, HRT can be an effective treatment. Any HRT regimen will provide bone benefits. The type of progestogen used does not have an impact on this.
What about vaginal or urinary symptoms?
For vaginal and urinary symptoms of the perimenopause and menopause, oestrogen can be administered directly into the vagina without the need for progesterone. Oestrogen is poorly absorbed into the rest of the body from the vagina, and so there are no associated risks of womb cancer when administered this way. Vaginal oestrogen can be used on its own, or can be combined with HRT taken to the whole body if vaginal or urinary symptoms are particularly troublesome and women could benefit from a ‘double dose’ of oestrogen in this area.
For how long should I take HRT?
Most symptoms of the menopause usually resolve with time, as the body adjusts to the low, constant level of oestrogen. Women may find that they do not need HRT for symptom control 5-10 years after the menopause, but decide to continue HRT for the bone and heart benefits it affords. The risk of breast cancer from HRT increases with age. The decision to continue HRT is an individual one and should be guided, but not dictated, by a clinician.
When I stop HRT, will my symptoms just return?
Taking HRT does not prevent the body from adjusting to lower levels of oestrogen. If symptoms do return on stopping, they will normally be less severe and last for a shorter duration. Gradually reducing the dose of HRT, before coming to a complete stop, can help.
What is ‘bio-identical HRT’ and is this available on the NHS?
‘Bio-identical HRT’ is a term used in the private sector to describe products which are advertised as being ‘tailor-made’ for individuals. They are combination hormone products, usually containing oestrogen, progesterone and sometimes testosterone. Products are made up with different quantities of hormones, and are advertised as meeting the individual needs of patients. An individual’s needs are reportedly determined by blood, saliva or urine tests.
The risks and benefits or products with varying quantities of hormones cannot be determined, and these products are unregulated, with limited safety information. As stated above, there is no evidence to suggest that products should be chosen based solely on blood, saliva or urine levels, as these levels vary greatly.
The term ‘bio-identical’ is sometimes confused with ‘body-identical’, but these term are not synonymous.
What about testosterone?
The female ovaries also produce testosterone, and the level of this hormone declines with age. The role of testosterone is less well understood but guidance does exist about its use in Hormone Replacement Therapy. Testosterone is principally use for the treatment of enduring low libido but is also thought to improve mood and cognition (thinking processes).
Oestrogen replacement also has an important role in improving libido, and for this reason it is recommended that oestrogen is replaced first, then the need for testosterone re-assessed.
Ensuring vaginal comfort with oestrogen replacement to the vagina, and the use of vaginal lubricants and/or moisturisers is also important. Sylk and YES are both trusted brands of intimate lubrication and moisturizers for women. These can be purchased online or are also available on prescription for some women.
We recommended that women also consider other factors that may be impacting on their libido and recommend the book Mind the Gap by Karen Gurney to further explore this.
I’ve heard there is a HRT shortage, why is that?
Recent increases in awareness of the benefits of HRT has resulted in an increase in demand. Other factors (such as the covid pandemic) also contribute to temporary supply issues. Pharmacies often don’t know when they will receive a delivery of HRT products if in short supply, and GP surgeries are not privy to the stock levels in individual pharmacies.
Patients can usually switch to an alternative product as a short term measure if their usual product is unavailable, and it is helpful if a patient has enquired with a number of pharmacies to source a supply, before asking the GP to redirect a prescription. The table below provides a rough estimate of the equivalent doses of products, allowing easy transitions from one to another if needed. Transitioning to an oral preparation from a transdermal one is associated with small additional risks, and this will usually require an appointment with a clinician to discuss a medication request.
Estradiol-approximate equivalent doses
Visit Women's Health Concern to view the factsheet on HRT: Types, doses and regimens
Oral
- Ultra Low: 0.5mg
- Low: 1.0mg
- Medium: 2.0mg
- High: 3mg to 4mg
Patch
- Ultra Low: Half 25mcg
- Low: 25mcg
- Medium: 50mcg
- High: 75 to 100mcg
Gel-Pump
- Ultra Low: Half a pump
- Low: 1 pump
- Medium: 2 pumps
- High: 3 to 4 pumps
Gel-sachet
- Ultra Low: Half of a 0.5mg Sachet = 0.25mg
- Low: 0.5mg
- Medium: 1mg to 1.5mg
- High: 2 to 3mg
Spray
- Ultra Low: 1 spray
- Low: 2 sprays
- Medium: 3 sprays
- High: not applicable
Other treatments
Antidepressants and other medication can have some benefits for hot flushes, and may be offered to women who have medical contraindications to taking HRT, or to women who do not wish to take HRT. These products do not provide any reduction in the risk of heart disease or bone thinning (osteoporosis).
Some women also find benefit from herbal remedies and increased dietary intake of oestrogen. These treatments are not well studied, their benefits are unclear, and the risks less well understood.
Visit Women's Health Concern to view the factsheet on Complementary and alternative therapies
Contraception and the menopause
For women whose periods stop before the age of 50 years, guidelines recommend continuing contraception for 2 years after the last period. In women who stop menstruating after the age of 50 years, contraception is required for 1 additional year.
In women who are not having regular bleeding due to the use of hormonal contraception, and who cannot determine when their natural cycle stops, it is recommended that contraception is continued until the age of 55 years. Sometimes a series of blood tests can be used sooner than this to determine whether the menopause has already occurred, and whether contraception can be stopped sooner.
Summary & Resources
Langley House is a menopause friendly practice with sufficient expertise amongst our staff to successfully manage symptoms or the perimenopause and menopause.
If you wish to have a consultation about the menopause or perimenopause, please contact the surgery. You may be asked to complete a questionnaire in the first instance to help us better meet your needs.
Whilst waiting for your appointment, please see below a list of trusted resources about the perimenopause and menopause. There is a wealth of information on the internet, but not all of it is evidence-based. The NHS provides treatment based on evidence, not opinion: some treatments recommended by private clinics or celebrities may not be available on the NHS.
- Rock My Menopause: Patient facing campaign of the Primary Care Women’s Health Forum
- Women's Health Concern: Patient facing campaign of the British Menopause Society
- Balance: Education resource from Dr Louise Newson, GP Menopause Specialist and Menopause Campaigner
